The Mighty's Ulcerative Colitis Condition Guide
Editor's Note
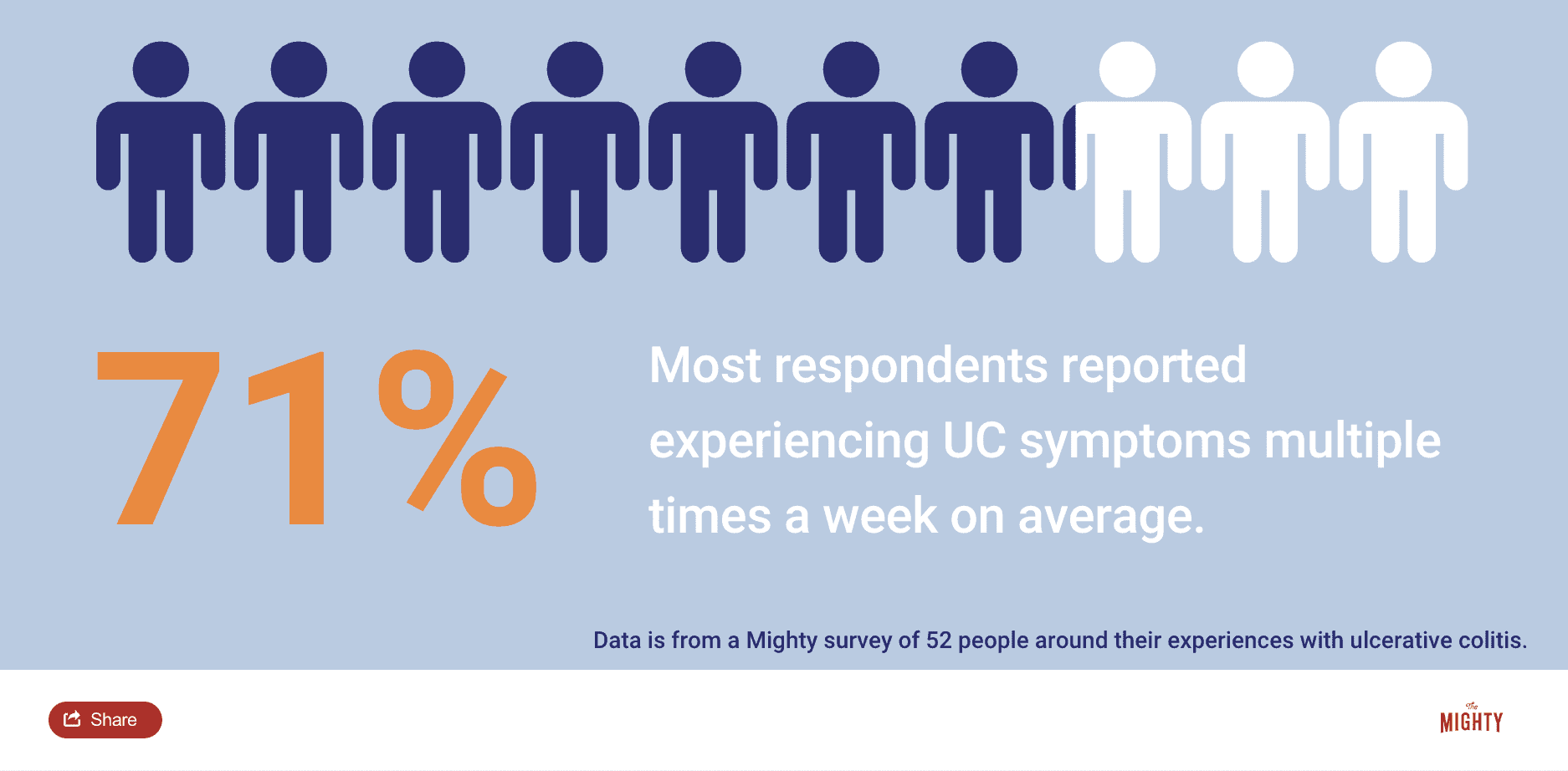
The Mighty’s educational content combines the expertise of both the medical and patient community to support you and your loved ones through your health journeys. For this ulcerative colitis (UC) condition guide, we interviewed two UC experts, read the latest studies and surveyed more than 50 people living with UC and their caregivers.
Ulcerative Colitis at a Glance:
- Ulcerative colitis (UC) is an autoimmune condition that primarily affects the colon.
- Approximately 1.3% of Americans live with inflammatory bowel disease (IBD), which includes UC.2 However, there are likely many more cases that go undiagnosed.
- There are many options for UC management, including medications, lifestyle changes and surgery.

Medically reviewed by Jordan Axelrad, M.D., MPH.
What is Ulcerative Colitis (UC)? | Common UC Misconceptions | UC Management | Mental Health and UC | How To Talk To Others About UC | How To Find a Health Care Provider for UC | How To Support Someone With UC | Join a Mighty Community for UC
What Is Ulcerative Colitis?
Ulcerative colitis (UC) is an immune-mediated disease that is classified as an inflammatory bowel disease, or IBD. Immune-mediated and autoimmune conditions develop when the body’s immune system mistakenly sees and attacks healthy cells in the body as if they are a threat like a virus or bacteria. Similar conditions include rheumatoid arthritis, celiac disease, Crohn’s disease and lupus.
For those living with UC, the immune system sees the large intestine, or colon, as a “foreign invader” when it’s not. So the immune system fights against the colon and its healthy cells, causing inflammation and the resulting symptoms associated with UC.
Symptoms of UC can include:
- Frequent, urgent bowel movements
- Diarrhea
- Bloody stools
- Abdominal pain
UC can also cause symptoms outside of your colon, such as:
- Arthritis in the wrists and fingers
- Eye redness
- Skin rashes
- Fatigue
- Weight loss
- Body pain
What Is the Difference Between Crohn’s Disease and Ulcerative Colitis?
Getting a UC diagnosis can sometimes be a long journey for patients. Another IBD condition, Crohn’s disease, is often on the radar for doctors who specialize in digestive disorders. Doctors may evaluate patients for both inflammatory bowel disease conditions.
You may be wondering: What are the differences between these two IBD conditions? The truth is, their symptoms can appear similar, and their treatments can overlap. They do, however, have differentiating characteristics that help a gastroenterologist identify which one you’re experiencing. Oftentimes these characteristics can only be seen by looking at the digestive tract itself.
Here are key differences between ulcerative colitis and Crohn’s disease:
- Crohn’s disease can affect the entire digestive tract, from the rectum to the mouth. UC only affects the colon.
- Individuals with Crohn’s disease might experience additional symptoms, such as mouth or gum ulcers, because of upper digestive tract inflammation.
- Crohn’s disease may affect the digestive tract differently than UC. Those living with Crohn’s disease can have healthy areas of the digestive tract in between inflamed areas called skip lesions, while people with UC often have continuous inflammation.
- UC can be diagnosed with a colonoscopy, while a Crohn’s diagnosis might include additional tests, such as an upper endoscopy or radiography.
- Complete remission tends to be more common with UC, if treated properly. Crohn’s disease remission can be more difficult to achieve.
How Ulcerative Colitis Is Diagnosed
To make a correct diagnosis, your doctor will use several tests to determine what areas of your digestive system are impacted. Doctors can see how much area of the digestive tract is affected through a colonoscopy (visual inspection of the large intestine through a camera) and an upper endoscopy (visual inspection of the upper digestive tract through a camera). Depending on your symptoms, a doctor might order other tests as well, such as imaging studies like radiography or an MRI as well as testing stool samples.
Getting a UC diagnosis can feel scary at first. If you’re feeling overwhelmed by a UC diagnosis, Mighty contributor Grady Stewart wants you to know that it’s OK:
“Allow yourself to process your diagnosis. A new diagnosis comes with a range of emotions. There’s no correct or incorrect to respond to such a life-changing event. Feeling sad, angry or anxious are all totally normal reactions to being diagnosed with a chronic condition. It’s also acceptable to feel undisturbed, or even relieved by a diagnosis. Recovery and acceptance are a process and not an end goal. Paying attention to your physical and mental health can help you figure out what makes living with ulcerative colitis easier, and what makes it harder. Ultimately, it does get easier.”
Read more about life with ulcerative colitis from fellow Mighties here:
- ‘The Ick’ of Ulcerative Colitis
- 10 Things This UC Patient Wants You to Know
- 6 Things Life with an Ostomy Isn’t
- 8 Tips to Make It Through the Grocery Store with UC

Common Ulcerative Colitis Misconceptions
One of the common misconceptions about ulcerative colitis (UC) is that it’s “just a bathroom disease.” People living with UC are definitely familiar with the toilet-related symptoms, as they are the main red flags that something’s not right. However, like many other chronic conditions, UC goes beyond the porcelain throne. UC can also affect body image, self-esteem, mental health, energy levels, weight and other aspects of wellness.
Inflammatory bowel disease, including UC, can also be confused with irritable bowel syndrome (IBS). While both present bathroom-related symptoms, they’re not the same. The main difference is IBS does not cause inflammation while IBD does. Doctors can observe signs of IBD in the digestive tract during testing, unlike with IBS.5
Another common myth is that UC is caused by poor diet choices. While there’s growing research around potential causes of the conditions, the truth is that there isn’t yet a known cause for UC.
Some people living with UC have also heard comments regarding weight loss, citing UC as an “easy” way to lose weight. While it’s true that weight loss is a common symptom of ulcerative colitis, it’s definitely not something that people with UC want to go through. This outlook can perpetuate body image struggles that many people face when living with UC.
To learn more about what people living with UC had to say about common UC misconceptions, we asked The Mighty community to share their experiences.
Here’s what they had to say:
- “Just because UC is an invisible illness doesn’t mean it’s not affecting me greatly. It plays a big role in my life.”
- “That it’s not just a bathroom disease, its impact on mental health, it’s not just a ‘stomach ache.’”
- “It is not just like IBS! UC affects much more of the body and [can] leave you feeling constantly ill.”
- “UC isn’t caused by a bad diet. There is no known cause. I follow a fairly good diet and have made changes to accommodate my UC, but my food didn’t cause it in the first place.”
- “People have said to me, ‘Aren’t you glad that you can lose weight easily?’ Obviously I’m not. It’s not just magically losing weight; it’s bloody diarrhea, vomiting, fatigue, lack of appetite and so many other things.”
- “Perhaps the biggest misconception about ulcerative colitis, and all other invisible illnesses, is that appearance is correlated with the severity of illness. In reality, this couldn’t be further than the truth.”
- “That there is no such thing as mind over matter. No amount of positivity or resilience will keep my intestines from churning if they’re flaring.”
- “When I have [to] go to the bathroom, I have [to] go! It’s [an] Emergency! I can not control it!”
You can also read stories about dealing with ulcerative colitis misconceptions here:
- What I Wish Others Knew About Life with UC
- To the People Who Tell Me I’m ‘Too Young’ to Be This Tired
- To Those Who Think IBD Is ‘Just a Bathroom Disease’

Ulcerative Colitis Management
An ulcerative colitis (UC) diagnosis can be daunting because it’s a chronic condition without a well known cause or cure. When diagnosed with a complex condition like ulcerative colitis, some may feel apprehensive about the treatment journey. You may be asking yourself:
- Is it really that bad that I need to try more “serious” medications?
- Will I have to have surgery?
- Will I ever be able to live a “normal” life?
The good news is that UC can often be managed with the help of a health care team, which usually includes a gastroenterologist (GI), a doctor who specializes in digestive disorders like UC. If you’re considering seeking help for UC symptoms, but are apprehensive about starting the process, Jordan Axelrad, M.D., MPH, an UC specialist, says:
“There are two reasons why you need to be treated. Number one: you need to feel better now. And then we want to prevent this from coming back.”
UC is a relapsing and remitting disease. That means there may be periods of time when symptoms are worse and others when they seem to disappear. It is important to manage UC not only when you’re experiencing symptoms, but continue managing the condition when you’re feeling better to prevent a relapse.
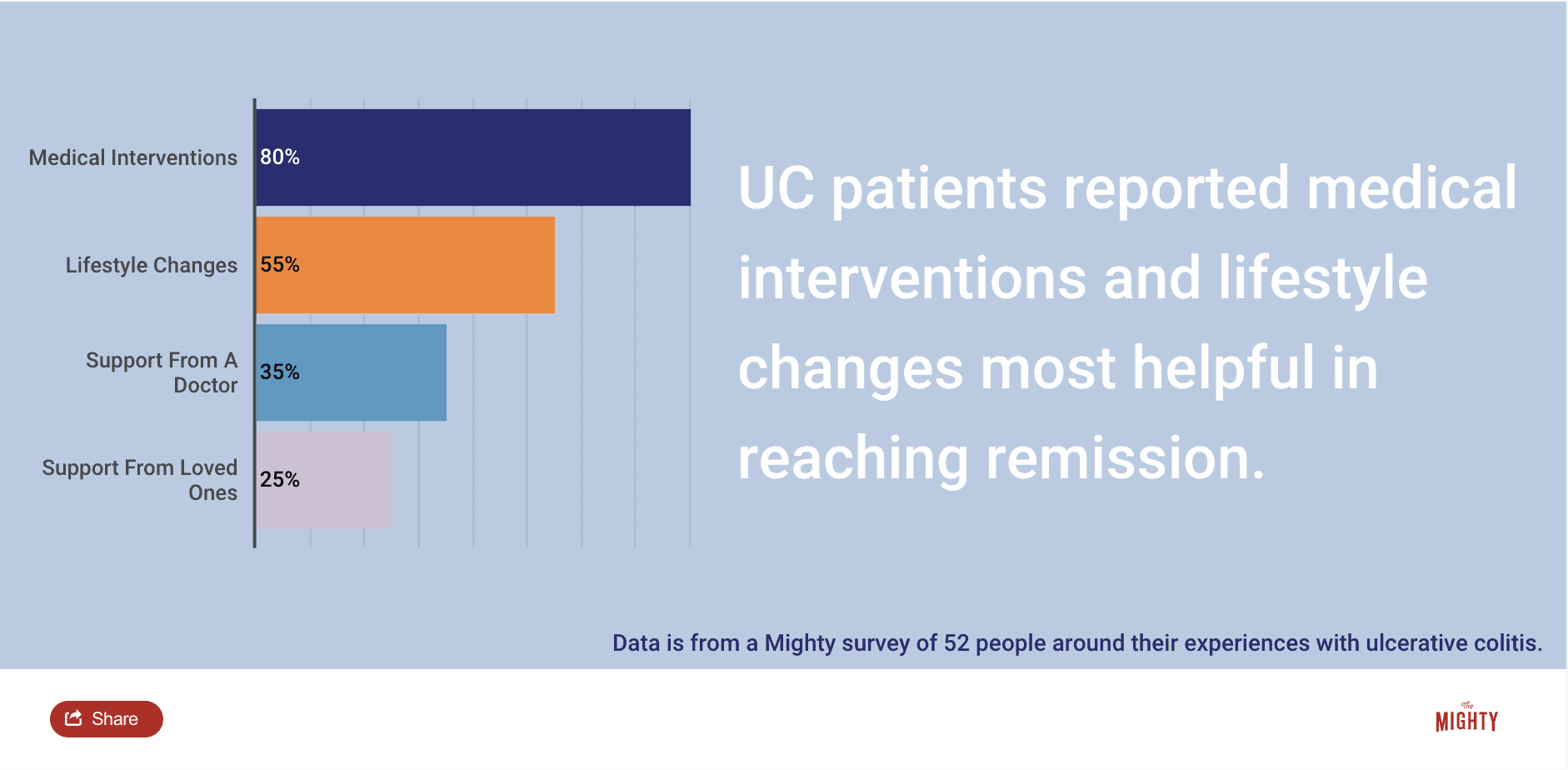
To help relieve ulcerative colitis symptoms and prevent them from getting worse or coming back, there are many different strategies and treatment options to explore with your health care team. Some of these options may include medication, surgical interventions and lifestyle changes.
Medications for UC often target inflammation in the body and the colon. Some medication types include:
- Aminosalicylates
- Corticosteroids
- Antibiotics
- Immunosuppressants
- Biologics
- JAK inhibitors
Sometimes, medications are not the best choice for managing UC and your GI may recommend surgical interventions. Rather than trying to reduce inflammation via medications, these surgical options remove the diseased areas of your colon altogether. Some surgical interventions you may hear about for UC include:
- Ostomies
- “J-pouch”
- Colectomy
No matter which options you and your doctor decide to try, it’s important to talk with your health care provider about the risks and benefits of different treatment options. You may feel apprehensive about more intensive options, like injections, infusions or surgery, than you’re comfortable with. However, it’s important to know these interventions are well-studied. Your GI specialist will recommend these options to help improve your quality of life and to prevent the damage living with untreated UC may cause. When left untreated, UC may contribute to other complications such as:
- Colon cancer
- Malnutrition
- More severe UC
- infections
- The need for more invasive surgical procedures
How To Build a Health Care Team for Ulcerative Colitis:
Creating a health care team that works for you is important in managing a chronic condition like UC. Do you have a gastroenterologist in your corner? Are you looking for a new primary care physician? Do you work with a therapist? It can feel daunting to find specialized treatment, and that’s why we’re breaking down who can be a key player on your health care team. No matter where you are on your treatment journey, we want you to know that you don’t have to build your care alone.
Here are some health care professionals that may be able to help:
- Primary care physician (PCP)
- General gastroenterologist (GI)
- GI Surgeon
- Nutritionist
- Mental health professional
You may be asking yourself if you really need an entire team to help manage your UC. But the truth is that each person on your health care team plays an important role. Managing a condition like UC can be complex and the ultimate goal of this team is to help improve your quality of life. You may have extended periods of time where all you need is your PCP but you’ll want the expertise and support from all of these professionals on hand if needed. It will not only help you get specialized help during a flare up, but also reduce stress when flare-ups happen because you know your team has your back.
What Does ‘Successful’ Management of Ulcerative Colitis Look Like?
So what does “successful” management” of UC look like anyway? In short: what success looks like will be different for every patient. Treatment goals should be discussed with your health care team. Overall, there are two key aspects of UC management that a GI specialist will strive for: symptom resolution and reducing inflammation.
At the end of the day, inflammation in the colon can cause long-term damage, even though reducing inflammation does not always correlate with less GI symptoms. This can be frustrating when remission doesn’t correspond with you feeling better right away. Tackling UC treatment is a balancing act between how you feel day-to-day and how your colon looks under a microscope. How you balance that will be unique to you.
Caitlyn Smith, The Mighty’s Crohn’s and Ulcerative Colitis Support Community Leader, says:
“For me, my UC is under control when I am on the same page as my doctor, I’m not experiencing active symptoms, I can exercise regularly, and my scopes don’t reveal any active UC. That’s my version of remission. However, I have friends who battle every day for just one good day. I think that successful treatment can have two different meanings: clinical remission and the patient’s definition. Those might be two different things, but they can both qualify as ‘successful.'”
A good GI doctor will work with you to make sure that what you’re experiencing day-to-day is validated and heard when considering treatment options. Gil Melmed, M.D.,MS, an ulcerative colitis specialist at Cedars-Sinai Medical Center wants you to know:
“People can have GI symptoms for a lot of reasons. Maybe their ulcerative colitis is healed with medications but they’re still having diarrhea, bloating, abdominal pain, etc. I think that it’s important to recognize that both healing of inflammation and symptom management are really important.”
On the flip side, treatments may have eliminated your GI symptoms — you’re feeling great! But that may not be a green light to say, “I no longer have active UC.” The only way to prove UC is in clinical remission is through testing like a colonoscopy or stool sample. That’s why many people who live with UC still get regular colonoscopies or may need additional therapies, despite no longer experiencing ulcerative colitis symptoms.
Other Ways To Manage Living With Ulcerative Colitis
Quality of life is an important factor in the decision-making process for UC treatment because the condition can interfere with daily life. For some people, that may be going to the bathroom more than usual, for others that may mean completely rearranging their schedule and being unable to enjoy life without significant planning. Incorporating self-care and lifestyle changes into your treatment plan may be helpful.
Self-Care Practices
Making self-care a priority may help you manage UC symptoms, particularly the stress and emotional toll living with a chronic condition. It’s important to incorporate many self-care techniques that appeal to you. For example, taking a bath not only calms the mind, but it can relax the gut too. Exercise is another great way to practice self-care, while also maintaining a healthy lifestyle. Sleep is an often overlooked self-care tactic, as many of us don’t get enough of it. A good night’s rest goes a long way in improving your mood and keeping your body on a regular schedule.
Nutrition
Another important part of UC management is nutrition. Because UC largely affects the colon, what we eat can greatly impact how our digestive system responds. Some people may notice that certain foods trigger symptoms and diets to take those foods into account may help. Some people may opt for a low-to-no gluten diet, while others may benefit from skipping dairy. UC may also affect your ability to digest food and absorb nutrients. Everyone is different, so it’s important to talk to your doctor about what works for you. Working with a nutritionist can help you find a balanced diet that works with you and your symptoms.
Symptom Tracking
Symptom tracking is an important part of ulcerative colitis management. The unpredictability of UC symptoms, particularly bathroom urgency, can cause people a lot of anxiety about even leaving their house. Where will the nearest bathroom be? However, by monitoring symptoms and noticing patterns, people living with UC can start to prepare for potential triggers ahead of time. Recognition of symptoms is an important step in managing any condition or disorder, which is why we created this UC-specific symptom tracker to help support your UC management journey:
To learn more about what management strategies have helped people living with ulcerative colitis, we reached out to the Mighty community.
Here’s what they had to say:
- “Build up your mental health toolkit whenever you have time. That could be finding peer support, a therapist or engaging in your favorite self-care activity.”
- “Take anything off your plate that’s not a ‘must.’”
- “Remember that it’s OK to say no. Over-exerting yourself, or entering a stressful situation you’d otherwise avoid, can trigger a flare-up of symptoms. Just say no.”
- “Be gentle with yourself. Some days are rough with UC, while others are better. Listen to your body.”
You can also find other management resources here:
- “Gotta Go” Resource Card from Girls With Guts
- Living with IBD: Pain and Fatigue
- The Best Bathroom Locator Apps
- Tips for Self-Advocacy from Girls With Guts
No matter where you’re at in your treatment journey, it’s important to know that your health care team, caretakers and community are an important source of support. It’s not easy managing a complex, chronic illness like UC, but that doesn’t mean you have to do it alone.

How To Talk To Others About Ulcerative Colitis
Talking about ulcerative colitis (UC) can be difficult, especially since it’s an invisible illness with bathroom-related symptoms. However, it’s important to feel comfortable talking about what you need and want to share about your UC experience, whether it’s with your doctor or a partner.
Talking To a Health Care Provider About Ulcerative Colitis Symptoms
It can feel uncomfortable talking about some of the symptoms you may be experiencing with UC. Discussing bowel movements, bloody stools, diarrhea, vomiting and “accidents” may not feel like a popular topic. However, it’s important to remember two things: these details are important to help manage your UC, and there’s nothing you can say that your doctor hasn’t heard before.
If it feels overwhelming at first, you’re not alone. It’s hard for many people to start those conversations for the first time, partly because many people are still nervous about what’s happening in their own bodies. However, it does get easier over time, and discussing embarrassing things now might prevent a flare-up down the line.
If you need a little bit of encouragement, Caitlyn Smith, The Mighty’s Crohn’s & Ulcerative Colitis Support community leader, wants you to know:
“There is nothing you can say to your GI or other doctors that they haven’t heard before. GIs specialize in diseases affecting the gastrointestinal tract, which means they spend their every day talking about digestion, bowel movements, ulcers and everything else associated with UC and IBD. They’ve heard it all, and I think it’s always best to take a deep breath and rip the bandaid off. A good doctor will support you and applaud your bravery in sharing something you felt embarrassed about.”
To help you navigate your next visit with a health care professional, we created a downloadable discussion guide. We hope this guide helps you get the most out of your appointments:
Ulcerative Colitis Health Care Provider Discussion Guide
Talking To Friends and Family About Ulcerative Colitis
There is no shame in talking about symptoms related to the bathroom; it’s part of the UC experience. That’s why we created this worksheet to help you confidently talk about your unique journey with ulcerative colitis. Feel free to doodle, jot down notes and use it in conversations with family, friends, loved ones, colleagues and others in your community.
Dating With Ulcerative Colitis
Being romantically involved with someone while living with UC can be… an interesting experience. On the one hand, it feels validating to meet someone who doesn’t run away when you first disclose your diagnosis. On the other hand, when is the best time to talk about UC? What about sleepovers that aren’t near your own bathroom? What if you pass gas in front of them? What if you feel urgency after a second-date dinner? Is sex going to be uncomfortable with UC?
The anxiety can feel overwhelming, but it’s possible to move through it when exploring the dating world with UC. Plus, if you’re looking for your lifelong partner, discussing hard things like a chronic condition can show them you’re comfortable with them. It can also show you if they’re in it for the long haul. Everyone, ulcerative colitis or not, is deserving of love and support from their partner, no matter what.
Angelica Catalano, Director of Social Impact at The Mighty who lives with UC, wants you to know:
“You don’t have to push yourself to date when you’re not ready. There are ways to socialize (and even date) virtually so you can dip your toe in without expending too much. There is no ‘right’ time to tell someone new you’re dating about your ulcerative colitis.”
If you feel like you need to hide your symptoms or are unsure if anyone will love all of you, UC included, Angelica shared this reminder:
“I tend to explain to others that living with UC has shaped me into who I am in a lot of positive ways — I’ve gained more empathy, and insight into myself as a person. It’s part of my story, so I don’t hide it. However, it doesn’t need to be the first thing I say when meeting someone new. That has helped me, so hopefully that helps people who are dating! I’m now married to someone who I was honest with early on, because I had very bad flares at the time. It helped me find out he was the real deal, to see how he dealt with my condition.”
You can read more about how other Mighties have navigated dating with invisible illness here:
- What I Forget to Ask My Fiancé as He Sits With Me When I’m in Pain
- The Challenges of Talking About My Ulcerative Colitis
- How Honest Should You Be When Hooking Up and Dating With an Ostomy?
- A Guide to Intimacy and Sex When Have Irritable Bowel Disease
Family Planning With Ulcerative Colitis
If you’re planning to start a family in the future, congratulations! Family planning with UC can present its own set of considerations, especially if the person giving birth has UC. You may be asking yourself these questions when first considering family planning with UC:
- Will your child develop ulcerative colitis?
- Will pregnancy cause a flare-up?
- Will a flare-up cause pregnancy complications?
- Is a C-section delivery the best way to go?
These are all great questions to discuss with both your OB-GYN and UC care team. In many cases, whether or not you’re experiencing a flare during conception can impact your pregnancy. Depending on your specific symptoms and other conditions you may have, this will be different for everybody. Your doctor will be able to walk you through what you should consider when you’re considering pregnancy, including the potential risks and solutions to ensure a healthy pregnancy and baby.
It’s also important to talk about what happens after the baby comes. Starting a family adds a lot of time-consuming tasks, sleepless nights and extra stress into the mix. And all of these things can trigger ulcerative colitis symptoms to flare. It’s always important to remain open and honest with your parenting partner(s), as well as raise your concerns with your health care team. Starting a family is a huge, exciting step, and it can be made easier by asking for support!

Mental Health and Ulcerative Colitis
Talking about UC and mental health is often overlooked when you’re considering how to manage your chronic illness. Just like a gastroenterologist helps keep your physical symptoms in check, a therapist or counselor can help address the emotional side effects of living with UC. Stress can be a major trigger for physical symptoms, so it’s important to pursue mental support during your ulcerative colitis journey.
One study found that more 80% of people living with UC also had a mental health diagnosis, from anxiety and depression to post-traumatic stress disorder (PTSD).1 Anxiety and depression are more common among people with UC, and can aggravate the disease itself.3,4 Anxiety, for example, can be related to your UC symptoms, especially around guaranteeing bathroom access at all times. Some people living with UC refer to it as the “cycle,” where you stress about symptoms, then symptoms flare up, then you stress about the flare-up.
Living with any medical condition can be a traumatic experience, including UC. Angelica Catalano, Director of Social Impact at The Mighty, shared her experience:
“I didn’t realize in recent years that I carry trauma from this illness. I was hospitalized at a very young age, 6. I’ve also had an emergency surgery later in life, which shook me. Leading up to it I had tried to be vocal about the pain, but was often dismissed. After that I started getting panic attacks every few months. I had to start therapy with a psychologist trained in working with IBD patients, and I also started medication to help. Together, they’ve helped me stop having panic attacks and reduce my overall anxiety.”
According to Jordan Axelrad, M.D., MPH, a UC specialist from NYU Langone Health, many people living with UC people may struggle with their body image. Whether it’s the result of surgery or weight fluctuations caused by ulcerative colitis symptoms, the changes in your body can be difficult. Caitlyn Smith, a Mighty community leader, shared her experience:
“I wrap mental health and body image together. A lot of my issues with anxiety and depression were connected to my issues with my body and how it looked and functioned. I felt unworthy and inadequate for a large chunk of my life following UC. I sometimes felt really helpless, especially when flaring. Then when I got back into remission, the flare fear impacted me mentally. I work hard every day to speak kindly to myself and have grace with myself.”
If you’re struggling with your mental health while living with UC, you’re not alone. Embarking on a journey to find support for your mental health is a great step for your overall wellness. For what it’s worth, you are beautiful and whole just as you are.
Here are some stories from Mighties who have been there:
- The Questions I Ask Myself When I Wonder If My Illness Was My Fault
- To the One Who Has Caused Me So Much Grief, My Ulcerative Colitis
- We Need to Talk About the Emotional Side of Ulcerative Colitis
How To Support Someone Living With Ulcerative Colitis
UC is an invisible illness that many still struggle to understand, including the people living with it. Therefore, it may be difficult to know how to support your loved one with UC.
Our first tip? Ask them questions! That’s the best way to learn about their unique experience with ulcerative colitis. Doing your own UC research is also a great step; educating yourself helps you grasp the basics of ulcerative colitis and how it can present itself.
At the end of the day, one of the best things you can do is show up. Your presence — whether it’s in person or virtually — says, “I may not fully understand your experience but I believe you and I’m here for you in whatever ways I can be.”
Mighty contributor Grady Stewart said it best:
“Having an invisible illness can make it exhausting to keep up the façade of feeling well, or to not believe that you’re not doing well. Having people in your support squad who understand this alleviates the fatigue of explaining this disconnect between the visible and invisible.”
For insight on living with an invisible illness and how to support someone experiencing UC, check out these Mighty stories:
- Why I’m Done Apologizing for My Invisible Illness
- Why I’m Making the Invisible Visible as Someone With Inflammatory Bowel Disease
- 5 Lessons I’ve Learned About Dealing With a Chronic Illness in the Workplace

Join an Ulcerative Colitis Support Community
If you live with UC and want to connect with other Mighties who’ve been there, check out The Mighty’s Crohn’s & Ulcerative Colitis Support Community. Join the conversation around UC, learn more about IBD resources and become part of a family who gets it.
To join the community, click here.

This UC condition guide was created with support from many Mighty contributors and medical experts. You can learn more about the individuals interviewed for the creation of this resource here:
- Jordan Axelrad, M.D., MPH
- Gil Melmed, M.D., MS
- Caitlyn Smith, Mighty community leader
- Grady Stewart, Mighty contributor
- Angelica Catalano, Director of Social Impact at The Mighty
And to the 52 Mighties who took our UC survey and the Mighty community members who answered prompts to help inform this resource, thank you!

Sources
1 Cawthorpe, D. (2015). Temporal Comorbidity of Mental Disorder and Ulcerative Colitis. The Permanente Journal, 52–57. https://doi.org/10.7812/tpp/14-120
2 Centers for Disease Control and Prevention. (n.d.). IBD, Crohn’s, UC Data and Statistics. Centers for Disease Control and Prevention (CDC). Retrieved February 3, 2021, from https://www.cdc.gov/ibd/data-statistics.htm#:%7E:text=Inflammatory%20Bowel%20Disease%20Prevalence%20(IBD,Crohn’s%20disease%20or%20ulcerative%20colitis)
3 Choi, K., Chun, J., Han, K., Park, S., Soh, H., Kim, J., Lee, J., Lee, H. J., Im, J. P., & Kim, J. S. (2019). Risk of Anxiety and Depression in Patients with Inflammatory Bowel Disease: A Nationwide, Population-Based Study. Journal of Clinical Medicine, 8(5), 654. https://doi.org/10.3390/jcm8050654
4 Crohn’s & Colitis Foundation. (n.d.-a). Depression and Anxiety. Retrieved February 3, 2021, from https://www.crohnscolitisfoundation.org/mental-health/depression-anxiety
5 Crohn’s & Colitis Foundation. (n.d.-b). IBS vs IBD. Retrieved February 3, 2021, from https://www.crohnscolitisfoundation.org/what-is-ibd/ibs-vs-ibd